Most people are familiar with conditions linked with obesity such as type 2 diabetes, sleep apnea, hypertension and arthritis. However, obese women may also develop hormonal problems such as polycystic ovarian syndrome (PCOS). The relationship between obesity and PCOS is complex and involves the influence of various genetic and environmental factors.
Understanding polycystic ovary syndrome
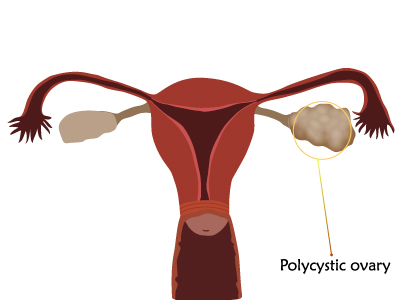
Polycystic ovary syndrome is a complex hormonal disorder that occurs in the women of reproductive age. To understand the condition, let’s understand normal reproductive process in females.
In a normal female, the ovaries contain fluid filled sacs called “ovarian follicles”, which contain an immature egg. These follicles continue to grow until ovulation. During ovulation, the follicles rupture to release a mature egg. Also, the ovaries produce estrogen and a small amount of the male hormone called “androgen”. Androgen can be produced by adrenal glands, fat cells, skin cells and ovaries.
In women with PCOS, the ovaries contain many partially formed follicles or “cysts”. These follicles rarely produce a mature egg, which may result in infertility. Additionally, excess of androgen is also produced which may result in development of facial hair or baldness.
The symptoms of PCOS vary from person to person but commonly include: irregular menstrual cycle, elevated levels of insulin or androgens and polycystic ovaries.
Development of PCOS
Many factors lead to the development of PCOS and some of them are discussed below
- Insulin resistance and production of androgens: Insulin resistance is a main factor that leads to the development of PCOS in women. Insulin resistance occurs when the body is unable to utilize the insulin properly. This leads in secretion of more insulin by the pancreas. The excessive production of insulin causes an increased production of the androgen by the ovaries.
- Hormones produced during fetal life: The condition may also be acquired during the fetal life. Excessive exposure of the fetus to androgens can promote a male pattern of distribution of abdominal fat, which increases the risk of insulin resistance and inflammation.
- Hereditary factors: It may be genetically inherited from the parents.
Relation between obesity and PCOS
Obesity and PCOS are interlinked i.e. obesity can cause PCOS and PCOS can lead to obesity.
In a healthy woman with PCOS, the condition results in insulin resistance that is independent of obesity. But, as insulin resistance increases appetite, it may make the woman to gain weight in the long run.
In obese women, insulin resistance and excess fat cells will result in elevated levels of androgens that may lead to the development of PCOS.
Further consequences
Obesity may increase the risk of the complications of PCOS such as:
- High blood pressure,
- Type 2 diabetes
- Sleep apnea
- Abnormal uterine bleeding
- Cholesterol problems
- Metabolic issues
- Problems in pregnancy.
What can be done?
When obese women have PCOS, reducing weight is imperative. Shedding even few kilograms can ease the symptoms of PCOS, help make periods regular and help manage blood sugar levels.
For reducing weight:
- Avoid processed or sugary foods and include fresh and natural foods rich in fibre such as whole wheat bread, brown rice, barley, etc.
- Try simple exercises such as walking. Regular physical activity helps with common health issues of both obesity and PCOS including sleep apnea.
Reducing weight can be a challenge for some obese women as they are used to sedentary lifestyle and are mostly confined to their homes. But efforts can be made by taking proper diet and performing basic exercises right at home, such as exercising on static cycle or treadmill. Even a moderate weight loss of 5-7 % throughout six months can lower insulin and androgen levels. It is also essential to quit smoking to lower the androgen levels.
When healthy diet and physical exercises doesn’t reduce weight, medications may also be prescribed to reduce hunger, manage diabetes or to improve the cholesterol levels. Surgery may be performed in severely obese women or when all the other methods have failed. The weight lost after a period of performing the surgery, helps regulate the menses and prevent diabetes along with other complications of obesity and PCOS.
Other issues related to PCOS can be tackled as follows:
- If fertility is an issue, then medications may be prescribed to improve ovulation and enable the release of a healthy egg. When medications have failed to work, assisted reproductive techniques such as in-vitro fertilisation serves as an alternative.
- To curb depression or anxiety, women can learn tai chi, yoga or acupuncture.
- To regularise menses and treat undesirable hair growth and acne, hormonal birth control medications may be prescribed.
References
https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/androgen-deficiency-in-women
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2861983/
https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/polycystic-ovarian-syndrome-pcos